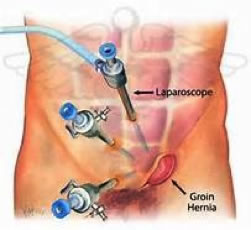
 Hernia repair refers to a surgical operation for the correction of a hernia (a bulging of internal organs or tissues through a defect in the wall of a body cavity). Hernia Repair Hernias can occur in many places, including the abdomen, groin, diaphragm, brain, and at the site of a previous operation. There are many different approaches to the surgical repair of hernias, including herniorrhaphy, hernioplasty, and herniotomy. Hernia repair is often performed as an ambulatory procedure.
Hernia repair refers to a surgical operation for the correction of a hernia (a bulging of internal organs or tissues through a defect in the wall of a body cavity). Hernia Repair Hernias can occur in many places, including the abdomen, groin, diaphragm, brain, and at the site of a previous operation. There are many different approaches to the surgical repair of hernias, including herniorrhaphy, hernioplasty, and herniotomy. Hernia repair is often performed as an ambulatory procedure.
 An intussusception is a medical condition in which a part of the intestine has invaginated into another section of intestine, similar to the way in which the parts of a collapsible telescope slide into one another. Intussusception This can often result in an obstruction. The part that prolapses into the other is called the intussusceptum, and the part that receives it is called the intussuscipiens.
An intussusception is a medical condition in which a part of the intestine has invaginated into another section of intestine, similar to the way in which the parts of a collapsible telescope slide into one another. Intussusception This can often result in an obstruction. The part that prolapses into the other is called the intussusceptum, and the part that receives it is called the intussuscipiens.
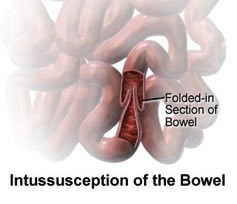 What causes intussusception? The exact cause of most cases of intussusception in children is not known. Intussusception It may happen after your child has infections of the nose, throat or bowel that are caused by a virus. Sometimes, an overgrowth of tissues in the intestines may become the place where the intussusception starts. These overgrowths may include a Meckel diverticulum, lymphoma, or an intestinal polyp. Diseases, such as Henoch-Schonlein purpura (HSP) and cystic fibrosis, may affect the bowel wall and increase risk of intussusception. Intussusception may also occur after your child has abdominal (belly) surgery.
What causes intussusception? The exact cause of most cases of intussusception in children is not known. Intussusception It may happen after your child has infections of the nose, throat or bowel that are caused by a virus. Sometimes, an overgrowth of tissues in the intestines may become the place where the intussusception starts. These overgrowths may include a Meckel diverticulum, lymphoma, or an intestinal polyp. Diseases, such as Henoch-Schonlein purpura (HSP) and cystic fibrosis, may affect the bowel wall and increase risk of intussusception. Intussusception may also occur after your child has abdominal (belly) surgery.
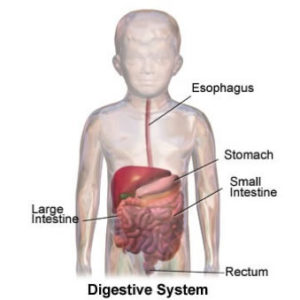
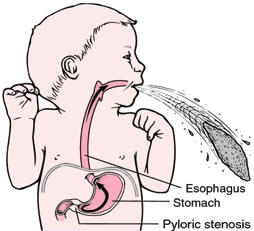 Pyloroplasty is surgery to widen the opening in the lower part of the stomach (pylorus) so that stomach contents can empty into the small intestine (duodenum). Pyloroplasty The pylorus is a thick, muscular area. When it thickens, food cannot pass through. The surgery is done while you are under general anesthesia (asleep and pain-free).
Pyloroplasty is surgery to widen the opening in the lower part of the stomach (pylorus) so that stomach contents can empty into the small intestine (duodenum). Pyloroplasty The pylorus is a thick, muscular area. When it thickens, food cannot pass through. The surgery is done while you are under general anesthesia (asleep and pain-free).
The surgeon makes a cut in the belly area. If the surgery is done using a laparoscope, three smaller cuts are made instead. The surgeon cuts through some of the thickened muscle so it becomes wider. The cut is then closed in a way that keeps the pylorus open. This allows the stomach to empty
 Pyloromyotomy is a surgical procedure in which an incision is made in the longitudinal and circular muscles of the pylorus. Pyloromyotomy It is used to treat hypertrophic pyloric stenosis. Hypertrophied muscle is cut along the whole length, till mucosa bulges out. If mucosa is injured, it is sutured horizontally using interrupted vicryl or silk sutures.
Pyloromyotomy is a surgical procedure in which an incision is made in the longitudinal and circular muscles of the pylorus. Pyloromyotomy It is used to treat hypertrophic pyloric stenosis. Hypertrophied muscle is cut along the whole length, till mucosa bulges out. If mucosa is injured, it is sutured horizontally using interrupted vicryl or silk sutures.
Stomach ache is a non-medical term used to describe various forms of nausea or abdominal pain. Stomach ache can be a symptom of many different maladies, from food poisoning to peptic ulcers.
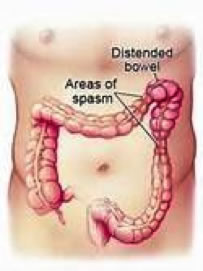
Irritable bowel syndrome (IBS) is a common disorder that may affect up to 30 percent of all Americans at some time during their lives. The disorder has many names, including nervous colon, spastic colon, spastic bowel, mucous colitis and spastic colitis. However, it should not be confused with diseases like ulcerative or Crohn’s colitis. IBS is a syndrome, a pattern of symptoms such as pain and bloating that tend to occur together. It is not a “disease” in the normal sense of the word (i.e., it cannot be caught or transmitted from person to person as a cold can nor can it be cured by an operation or medication). It is not life threatening.
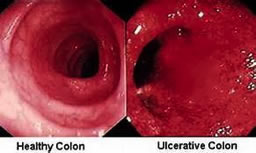 Ulcerative colitis is the technical term for what many know as inflammation of the colon. Obstruction of the Colon It is considered to be an inflammatory bowel disease (IBD), a general term given for more than one type of bowel disorders. Ulcerative colitis causes inflammation and sores to form on the lining of the colon and rectum, resulting in bleeding and frequent diarrhea. This condition can occur in anyone, usually beginning between the ages of 15 and 30. The treatment varies according to the severity of the person’s condition and ranges from the use of medication to surgery.
Ulcerative colitis is the technical term for what many know as inflammation of the colon. Obstruction of the Colon It is considered to be an inflammatory bowel disease (IBD), a general term given for more than one type of bowel disorders. Ulcerative colitis causes inflammation and sores to form on the lining of the colon and rectum, resulting in bleeding and frequent diarrhea. This condition can occur in anyone, usually beginning between the ages of 15 and 30. The treatment varies according to the severity of the person’s condition and ranges from the use of medication to surgery.
 Anal fistula, or fistula-in-ano, is an abnormal connection between the epithelialised surface of the anal canal and (usually) the perianal skin. Anal fistulae originate from the anal glands, which are located between the two layers of the anal sphincters and which drain into the anal canal. If the outlet of these glands becomes blocked, an abscess can form which can eventually point to the skin surface. The tract formed by this process is the fistula You can get a fistula as a result of an infection or an abscess (collection of pus). It can also be caused by conditions that affect the bowel such as Crohn’s disease. If you are diagnosed with a fistula, you will also be tested for Crohn’s, as unfortunately the two go hand in hand. Crohn’s sufferers are more prone to developing fistulas.
Anal fistula, or fistula-in-ano, is an abnormal connection between the epithelialised surface of the anal canal and (usually) the perianal skin. Anal fistulae originate from the anal glands, which are located between the two layers of the anal sphincters and which drain into the anal canal. If the outlet of these glands becomes blocked, an abscess can form which can eventually point to the skin surface. The tract formed by this process is the fistula You can get a fistula as a result of an infection or an abscess (collection of pus). It can also be caused by conditions that affect the bowel such as Crohn’s disease. If you are diagnosed with a fistula, you will also be tested for Crohn’s, as unfortunately the two go hand in hand. Crohn’s sufferers are more prone to developing fistulas.
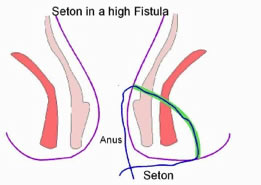 Fistulas most often occur as a result of one or more perianal abcesses. A perianal fistula is a collection of pus under the skin next to the anal canal (back passage). It is usually caused by an infection of the glands of the anal canal. This presents as a painful lump in the area and may be associated with a fever. The treatment involves drainage of the pus usually by operation. Some of these infections go on to form a longstanding fistula (a track running from the skin near the anus to the inside of the anal canal). These intermittently swell and discharge pus and blood. The treatment involves surgery to either open the track to the skin or close the inside opening. In laymans terms, a fistula is a tunnel that connects two organs or vessels that normally wouldn’t be connected. The fistulas need to be treated and closed off with surgery. There are different techniques used in surgery to do this. But before a fistula can be closed off, it needs to be kept open to ensure that all infection and pus from the abcesses has been drained. To keep the fistula open, surgeons will insert a seton under general anesthetic. A seton is a surgical cord that is run into the fistula opening, through the fistula track, out the anus and then tied together, so essentually it runs around in a loop. This stops the fistula opening closing up and allows the pus to drain out over time so that there is no longer any infection inside the fistula.
Fistulas most often occur as a result of one or more perianal abcesses. A perianal fistula is a collection of pus under the skin next to the anal canal (back passage). It is usually caused by an infection of the glands of the anal canal. This presents as a painful lump in the area and may be associated with a fever. The treatment involves drainage of the pus usually by operation. Some of these infections go on to form a longstanding fistula (a track running from the skin near the anus to the inside of the anal canal). These intermittently swell and discharge pus and blood. The treatment involves surgery to either open the track to the skin or close the inside opening. In laymans terms, a fistula is a tunnel that connects two organs or vessels that normally wouldn’t be connected. The fistulas need to be treated and closed off with surgery. There are different techniques used in surgery to do this. But before a fistula can be closed off, it needs to be kept open to ensure that all infection and pus from the abcesses has been drained. To keep the fistula open, surgeons will insert a seton under general anesthetic. A seton is a surgical cord that is run into the fistula opening, through the fistula track, out the anus and then tied together, so essentually it runs around in a loop. This stops the fistula opening closing up and allows the pus to drain out over time so that there is no longer any infection inside the fistula.
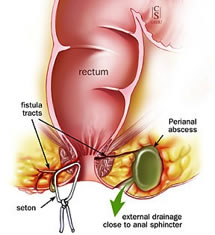 If you have a ‘shallow’ fistula that is close to the surface of the skin and doesn’t run through any muscle, the surgeons are usually able to tighten the seton over time until it eventually comes out altogether as the fistula heals. However, if you have a more complicated fistula that runs through muscle and is not close to the surface, you will then need corrective surgery. Fistula sufferers live each day with the seton in their body. You could even have more than one seton, depending on how many fistulas you have. At first they are difficult to live with, it can be uncomfortable to sit down, walk and go to the toilet. However, like everything, you will get used to living with a seton and will work out your own ways to deal with it. There are some tips on living with setons on the ‘ Tips and Advice’ page.
If you have a ‘shallow’ fistula that is close to the surface of the skin and doesn’t run through any muscle, the surgeons are usually able to tighten the seton over time until it eventually comes out altogether as the fistula heals. However, if you have a more complicated fistula that runs through muscle and is not close to the surface, you will then need corrective surgery. Fistula sufferers live each day with the seton in their body. You could even have more than one seton, depending on how many fistulas you have. At first they are difficult to live with, it can be uncomfortable to sit down, walk and go to the toilet. However, like everything, you will get used to living with a seton and will work out your own ways to deal with it. There are some tips on living with setons on the ‘ Tips and Advice’ page.
An anal fissure is a small tear in the lining of the anus, which can cause pain, bleeding and /or itching.
Cancer is known medically as a malignant neoplasm, is a broad group of diseases involving unregulated cell growth. In cancer, cells divide and grow uncontrollably, forming malignant tumors, and invading nearby parts of the body. The cancer may also spread to more distant parts of the body through the lymphatic system or bloodstream.
Often described as “varicose veins of the anus and rectum”, hemorrhoids are enlarged, bulging blood vessels in and about the anus and lower rectum. There are two types of hemorrhoids: external and internal, which refer to their location. External (outside) hemorrhoids develop near the anus and are covered by very sensitive skin. If a blood clot develops in one of them, a painful swelling may occur. The external hemorrhoid feels like a hard, sensitive lump. It bleeds only if it ruptures. Internal (inside) hemorrhoids develops within the anus beneath the lining. Painless bleeding and protrusion during bowel movements are the most common symptom. However, an internal hemorrhoid can cause severe pain if it is completely “prolapsed” – protrudes from the anal opening and cannot be pushed back inside.
Diverticula are pockets or pouches that develop through weaknesses in the colon wall, usually in the sigmoid or left colon, but may involve the entire colon. Diverticulitis describes perforation or inflammation of the diverticulum
Colectomy consists of the surgical resection of any extent of the large intestine (colon).
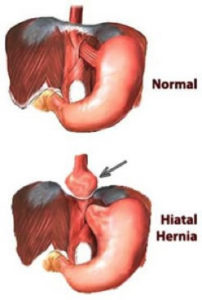 A hiatal hernia occurs through the diaphragm (or breathing muscle, which separates the chest from the abdomen) at the site where the esophagus (food pipe) normally goes through to attach to the stomach. In a hiatal hernia, the stomach bulges up into the chest through that opening. Patients with a hiatal hernia may have no symptoms. Often, however, patients have heartburn or GERD. Occasionally, patient can have chest pain.
A hiatal hernia occurs through the diaphragm (or breathing muscle, which separates the chest from the abdomen) at the site where the esophagus (food pipe) normally goes through to attach to the stomach. In a hiatal hernia, the stomach bulges up into the chest through that opening. Patients with a hiatal hernia may have no symptoms. Often, however, patients have heartburn or GERD. Occasionally, patient can have chest pain.
Chronic heartburn, which is usually a symptom of gastro-esophageal reflux disease or GERD. It is due to the acid from the stomach refluxing up into the esophagus. It is often frequent enough to have a significant impact on the individual’s quality of life by keeping him from enjoying certain foods or even keeping him up at night. It can also sometimes lead to serious conditions such as asthma, burning of the esophagus (esophagitis), and even cancer of the esophagus.
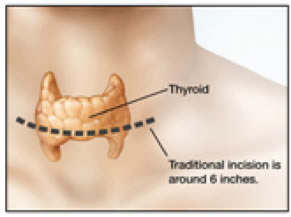 A thyroidectomy is a surgical procedure designed to remove all or part of the thyroid gland. Thyroid Thyroidectomies are used to treat thyroid cancer, severe hyperthyroidism (Grave’s disease), or an enlarged thyroid (goiter). There are 3 different types of thyroidectomy surgery. A Total Thyroidectomy, used for aggressive cancer, goiter, and hyperthyroidism, removes the entire thyroid. A Subtotal or Partial Thyroidectomy removes half of the thyroid, and is used for treating localized (isolated) or less aggressive cancers. A Thyroid Lobectomy removes approximately ¼ of the gland, and is relatively rare. During a thyroidectomy, the surgeon makes an incision across the base of the front of the neck. The surgeon separates the trachea and the parathyroid from the thyroid, and removes the necessary part of the gland. Patients usually return to normal activities in one week.
A thyroidectomy is a surgical procedure designed to remove all or part of the thyroid gland. Thyroid Thyroidectomies are used to treat thyroid cancer, severe hyperthyroidism (Grave’s disease), or an enlarged thyroid (goiter). There are 3 different types of thyroidectomy surgery. A Total Thyroidectomy, used for aggressive cancer, goiter, and hyperthyroidism, removes the entire thyroid. A Subtotal or Partial Thyroidectomy removes half of the thyroid, and is used for treating localized (isolated) or less aggressive cancers. A Thyroid Lobectomy removes approximately ¼ of the gland, and is relatively rare. During a thyroidectomy, the surgeon makes an incision across the base of the front of the neck. The surgeon separates the trachea and the parathyroid from the thyroid, and removes the necessary part of the gland. Patients usually return to normal activities in one week.
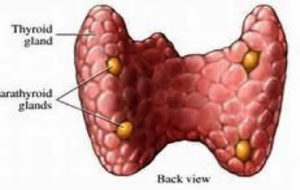 Minimally Invasive Radioguided Parathyroidectomy (or “MIRP”) is a newer surgical procedure designed to remove parathyroid tumors. Parathyroid The first step of a MIRP procedure involves injecting the four parathyroid glands with a small dose of a radioactive drug. A small geiger counter is then used to detect the hyperactive parathyroid gland or glands (which absorb radioactivity). The surgeon can utilize a small incision on a limited area of the neck to quickly locate and remove the affected gland rather than using a long incision that involves the entire neck and examining all 4 glands. The MIRP technique saves time (an average surgery lasts about one hour), results in less pain, shorter recovery time, and a higher cure rate than a traditional parathyroidectomy surgery.
Minimally Invasive Radioguided Parathyroidectomy (or “MIRP”) is a newer surgical procedure designed to remove parathyroid tumors. Parathyroid The first step of a MIRP procedure involves injecting the four parathyroid glands with a small dose of a radioactive drug. A small geiger counter is then used to detect the hyperactive parathyroid gland or glands (which absorb radioactivity). The surgeon can utilize a small incision on a limited area of the neck to quickly locate and remove the affected gland rather than using a long incision that involves the entire neck and examining all 4 glands. The MIRP technique saves time (an average surgery lasts about one hour), results in less pain, shorter recovery time, and a higher cure rate than a traditional parathyroidectomy surgery.
 The Anterior Approach for total hip replacement is a tissue-sparing alternative to traditional hip replacement surgery that provides the potential for less pain, faster recovery and improved mobility because the muscle tissues are spared during the surgical procedure. The technique allows the surgeon to work between your muscles and tissues without detaching them from either the hip or thighbones – sparing the tissue from trauma.
The Anterior Approach for total hip replacement is a tissue-sparing alternative to traditional hip replacement surgery that provides the potential for less pain, faster recovery and improved mobility because the muscle tissues are spared during the surgical procedure. The technique allows the surgeon to work between your muscles and tissues without detaching them from either the hip or thighbones – sparing the tissue from trauma.
Breast cancer is a type of cancer originating from breast tissue, most commonly from the inner lining of milk ducts or the lobules that supply the ducts with milk. Cancers originating from ducts are known as ductal carcinomas, while those originating from lobules are known as lobular carcinomas. Breast cancer occurs in humans and other mammals. While the overwhelming majority of human cases occur in women, male breast cancer can also occur. Surgery provides the single largest benefit, and to increase the likelihood of cure, several chemotherapy regimens are commonly given in addition
 An inferior vena cava filter (IVC filter) is a type of vascular filter, a medical device that is implanted by interventional radiologists or vascular surgeons into the inferior vena cava to presumably prevent life-threatening pulmonary emboli. Their effectiveness and safety profile is not well established, and in general, they are only recommended in some high-risk scenarios.
An inferior vena cava filter (IVC filter) is a type of vascular filter, a medical device that is implanted by interventional radiologists or vascular surgeons into the inferior vena cava to presumably prevent life-threatening pulmonary emboli. Their effectiveness and safety profile is not well established, and in general, they are only recommended in some high-risk scenarios.
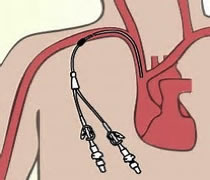
Long-term central venous access (LTCVA) plays a critical role in the management of cancer patients. Such LTCVA devices are particularly important in providing a reliable venous route for successful administration of multi-drug anticancer chemotherapy regimens and for various aspects of therapeutic and supportive care during bone marrow transplantation. Placement of LTCVA devices not only enables delivery of these complex therapeutic regimens, but it can also dramatically improve cancer patients’ quality of life
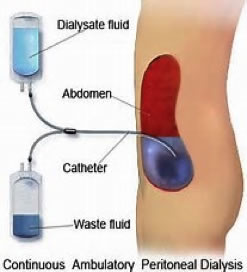 Peritoneal dialysis is a treatment for patients with severe chronic kidney disease. The process uses the patient’s peritoneum in the abdomen as a membrane across which fluids and dissolved substances (electrolytes, urea, glucose, albumin and other small molecules) are exchanged from the blood.
Peritoneal dialysis is a treatment for patients with severe chronic kidney disease. The process uses the patient’s peritoneum in the abdomen as a membrane across which fluids and dissolved substances (electrolytes, urea, glucose, albumin and other small molecules) are exchanged from the blood.
Hemodialysis is a method that is used to achieve the extracorporeal removal of waste products such as creatinine and urea and free water from the blood when the kidneys are in a state of renal failure.
A gastrectomy is a partial or full surgical removal of the stomach. Gastrectomies are performed to treat cancer and perforations of the stomach wall.
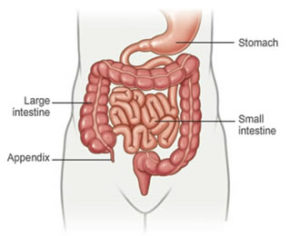 Appendectomy is the surgical removal of the vermiform appendix.This procedure is normally performed as an emergency procedure, when the patient is suffering from acute appendicitis.
Appendectomy is the surgical removal of the vermiform appendix.This procedure is normally performed as an emergency procedure, when the patient is suffering from acute appendicitis.
Cholecystectomy is the surgical removal of the gallbladder. It is a common treatment of symptomatic gallstones and other gallbladder conditions. Surgical options include the standard procedure, called laparoscopic cholecystectomy, and an older more invasive procedure, called open cholecystectomy.
Splenectomy is a surgical procedure that partially or completely removes the spleen. The spleen, similar in structure to a large lymph node, acts as a blood filter. Current knowledge of its purpose includes the removal of old red blood cells and platelets, and the detection and fight against certain bacteria.
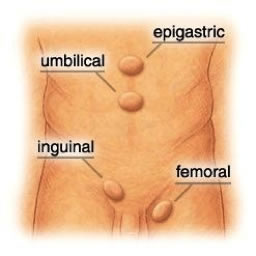 Hernia repair is a surgical operation for the correction of a hernia (a bulging of internal organs or tissues through a defect in the wall of a body cavity). Hernias can occur in many places, including the abdomen, groin, diaphragm, brain, and at the site of a previous operation. There are many different approaches to the surgical repair of hernias, including herniorrhaphy, hernioplasty, and herniotomy. Hernia repair is often performed as an ambulatory procedure.
Hernia repair is a surgical operation for the correction of a hernia (a bulging of internal organs or tissues through a defect in the wall of a body cavity). Hernias can occur in many places, including the abdomen, groin, diaphragm, brain, and at the site of a previous operation. There are many different approaches to the surgical repair of hernias, including herniorrhaphy, hernioplasty, and herniotomy. Hernia repair is often performed as an ambulatory procedure.
A tumor is defined as a swelling or morbid enlargement. Although often used as a synonym for neoplasm, the word tumor is not synonymous with cancer; tumors may be benign (non-cancerous), pre-malignant or malignant (cancerous), or can signify a lesion with no cancerous potential. A tumor results from an overabundance of cell growth and division; normally cells grow and divide to produce new cells in a controlled and orderly manner. In malignant tumors (that is, cancerous tumors), cells are abnormal and divide uncontrollably and without order. Often these cells spread to and damage nearby tissue and may spread to other parts of the body (metastases). Tumors vary in type and size, and the type of tissue they occur in often signifies their shape and how they grow.